What a Small Gesture Reveals About Presence, Power, and the Work We’re Actually Doing
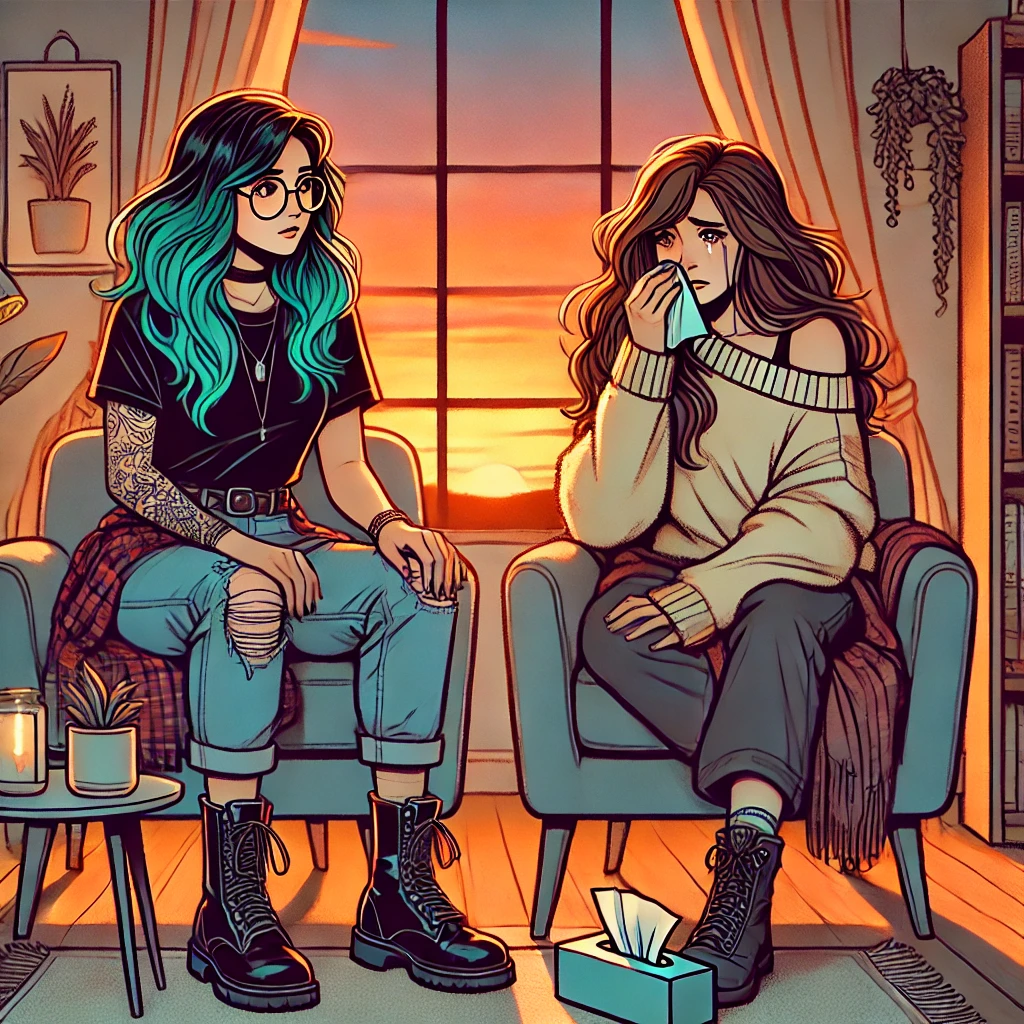
There is a moment every therapist knows.
The room is quiet. The air feels slightly heavier. A client’s voice cracks and then gives way. Tears arrive, sometimes tentatively, sometimes all at once. Somewhere nearby, a box of tissues waits. Innocent. Unassuming. Loud with implication.
This is the moment that launches a thousand supervision conversations.
Do you hand the tissue or not?
Do you wait?
Do you say something?
Do you stay silent?
Do you risk doing the “wrong” thing?
For something so small, the tissue has an outsized reputation in psychotherapy. It becomes a symbol, a litmus test, a quiet referendum on whether we are being attuned, cold, rescuing, withholding, or just plain awkward.
But the real question isn’t about tissues.
The real question is what we believe about emotion, presence, and our role when a client is visibly undone in front of us.
This post is not an argument for one “correct” response. It’s an invitation to slow down and look more closely at what is actually happening in the room when tears appear. Because when a client cries, something important has already shifted. And how we respond, even in the smallest ways, becomes part of the story the nervous system remembers.
Crying Is Not a Clinical Emergency
Let’s start by removing the invisible alarm bell.
A client crying in session does not mean the session has gone off the rails. It does not mean you have pushed too far, lost control, or failed to contain the work. It does not mean something needs to be immediately fixed, soothed, or redirected.
Crying is not a rupture. It is not regression. It is not evidence that therapy has become unsafe.
In many cases, it is the opposite.
Crying is a common human nervous system response. It shows up when emotion has enough space to move instead of being managed, intellectualized, or swallowed whole. For some clients, especially those who have spent a lifetime staying composed, competent, or “fine,” tears don’t appear until safety has already been established.
We absorb so many unspoken messages about crying, even as therapists. That it’s disruptive. That it derails productivity. That it needs to be contained quickly so the work can continue. As if the work isn’t happening precisely because the tears arrived.
When we treat crying like an emergency, we often do so out of our own discomfort. The urgency to intervene, explain, reassure, or tidy is understandable. But urgency communicates something. It suggests that this level of feeling is too much. That it needs to be managed to be allowed.
Therapy asks something different of us.
It asks us to recognize that emotion is not the enemy of progress. Often, it’s the doorway. Tears are not a mess to clean up. They are a signal that the nervous system is doing something meaningful, even if it’s uncomfortable to witness.
Before we debate what to do with our hands or the tissue box, we have to start here. Crying is not a problem to solve. It is a human process unfolding in real time.
And once we understand what crying actually does in the body, the rest of the conversation begins to shift.
What Crying Actually Does for the Nervous System
Before we decide how to respond to tears, it helps to understand what tears are actually doing.
Crying is not just an emotional expression. It is a physiological process involving the nervous system, the endocrine system, and the relational brain. When a client cries, their body is not malfunctioning. It is participating in a complex regulatory sequence that has been shaped by evolution, attachment, and survival.
Emotional tears are chemically distinct from reflex tears. They carry different information, and they often arrive at specific moments in the nervous system’s arc from activation toward release.
One of the most cited chemicals in emotional crying is cortisol, the body’s primary stress hormone. Cortisol has been found in higher concentrations in emotional tears, which has led researchers to hypothesize that crying may be one way the body metabolizes stress rather than simply holding it indefinitely. This does not mean crying “gets rid of” stress or solves the underlying problem. It means the system is reducing pressure. A valve opens. Something moves.
This matters clinically. When we rush to stop tears, we may be interrupting a process the body has been preparing for far longer than the session itself.
Crying is also associated with increases in oxytocin, a hormone involved in bonding, soothing, and feelings of safety. Oxytocin is particularly relevant in therapy because it is not just released internally. It is shaped relationally. Crying in the presence of a regulated, attuned other can amplify oxytocin’s effects, reinforcing the experience of being seen and not abandoned while vulnerable.
This is one of the reasons crying alone can feel different from crying with someone trustworthy. The chemistry changes when there is a witness.
Then there are endorphins, the body’s natural pain modulators. Endorphins can increase following emotional crying, contributing to the sense of relief, grounding, or softening that some clients describe afterward. Not joy. Not resolution. Relief. A slight easing of the edge that allows the nervous system to settle into a quieter state.
You may also see references to prolactin, a hormone linked to emotional expression and regulation. Prolactin levels tend to be higher in people who cry more frequently, which helps normalize crying as an individual difference rather than a deficit. Some nervous systems use tears more readily as a regulatory pathway. Others don’t. Neither is inherently healthier.
From a nervous system standpoint, crying is often tied to parasympathetic activity. Acetylcholine, a neurotransmitter associated with the parasympathetic system, plays a role in activating the lacrimal glands that produce tears. This is important because it challenges the idea that crying represents “loss of control.” In many cases, it reflects the body shifting out of sustained vigilance into a state where release becomes possible.
There is also ACTH, part of the stress-response cascade that helps regulate cortisol production. Its presence reinforces that crying is woven directly into the stress system, not separate from it. Tears are not an emotional afterthought. They are part of how the system recalibrates under load.
Put simply, crying often marks a transition. From holding to releasing. From guarding to allowing. From surviving to processing.
For many clients, especially those who are highly intellectual, competent, or accustomed to self-containment, tears do not signal dysregulation. They signal safety. The body is finally exhaling.
This is why treating crying as something to quickly soothe, redirect, or manage can be counterproductive. When we interrupt tears too soon, we risk cutting short a regulatory sequence that the nervous system rarely gets permission to complete.
Therapy does not need to manufacture crying. But when it appears, our role is not to hurry it along or shut it down. Our role is to protect the conditions that allow it to unfold safely.
Once we understand crying as physiology and regulation rather than failure or fragility, the next layer becomes impossible to ignore.
Crying does not happen in a vacuum.
It happens in context.
And context shapes meaning.
A Brief Cultural and Contextual Pause
Before we talk about what tears mean in the therapy room, we have to acknowledge something obvious and often overlooked.
Crying does not mean the same thing everywhere.
For some clients, tears were allowed, tended to, even welcomed. For others, crying was dangerous. It invited ridicule, punishment, withdrawal, or silence. Some learned early that tears made things worse, not better. Others learned that tears were the only way to be noticed at all.
Culture, family systems, gender expectations, race, religion, disability, and survival context all shape how crying is experienced and interpreted. Who was allowed to cry without consequence. Who had to stay composed to remain safe. Who learned that strength meant emotional containment. Who learned that vulnerability cost too much.
These meanings do not disappear when a client walks into therapy. They arrive quietly, layered beneath the present moment, shaping how tears feel in the body long before the therapist responds.
This is why it’s not enough to say “crying is good” without context. For some clients, that statement lands as permission. For others, it lands as pressure. As if there is now a correct emotional response they are failing to produce.
A culturally responsive stance asks us to stay curious rather than prescriptive. What does crying mean to this person? What did tears cost them historically? What rules were formed around emotional expression long before this room existed?
When a client cries, they are not just expressing emotion. They are crossing an internal boundary that was shaped by lived experience. Our job is not to assume what that crossing signifies, but to honor the courage it often takes to step there at all.
Therapists’ own cultural identities and emotional socialization also shape how these moments unfold. What feels supportive, neutral, or intrusive is never formed in a vacuum on either side of the room.
This pause matters because it keeps us from romanticizing tears. Crying can be regulating, but it can also be complicated, loaded, and layered with meaning that deserves respect rather than assumption.
Which brings us to another essential layer of nuance.
Not every nervous system experiences crying the same way.
A Trauma-Informed and Neurodivergent Lens
For some clients, crying does not feel like relief.
It feels overwhelming. Disorganizing. Flooding. It may come with shame, sensory overload, shutdown, or a sense of losing footing rather than finding it. This is especially true for clients with trauma histories, neurodivergent nervous systems, or long-standing experiences of emotional invalidation.
For these clients, crying may not yet be a regulatory experience. It may be something the body learned to avoid because it once led to harm, chaos, or abandonment.
This does not make crying bad. It makes safety unfinished.
Crying becomes regulating when the nervous system believes it will not be punished, dismissed, or left alone in the experience. That belief is not cognitive. It is earned through repeated moments of attuned presence over time.
For neurodivergent clients, sensory sensitivity can also shape how crying is experienced. The physical sensations of tears, changes in breathing, facial tension, or vocal shifts may be uncomfortable or destabilizing. Emotional expression that looks familiar to a therapist may feel internally disorienting to the client.
A trauma-informed, neurodivergent-affirming stance does not assume that crying is the goal. It assumes that choice and capacity matter. Regulation is not about producing tears. It is about expanding what the nervous system can tolerate safely.
This is where therapists can unintentionally get it wrong by overvaluing visible emotion. Tears are not the measure of depth. They are one of many expressions of processing. Stillness, numbness, anger, humor, intellectual reflection, and embodied awareness all belong here too.
The work is not to elicit crying. The work is to create enough safety that whatever response emerges can be met without urgency or judgment.
When crying does appear, especially for clients who rarely allow it, the moment is delicate. Not fragile, but meaningful. And what we do next carries weight.
Which brings us back to the object sitting quietly in the room.
Why the Tissue Is Never Just a Tissue
On the surface, a tissue is a practical object.
Tears happen. Faces get wet. Noses run. Hygiene matters.
And yet, in the therapy room, the tissue is never neutral.
It sits there quietly, doing nothing, until the moment it does everything. Once tears appear, the tissue becomes a symbol, whether we want it to or not. It carries meaning far beyond its intended use. It becomes a gesture. A message. A signal that the client’s nervous system is already decoding before words catch up.
Handing a tissue can communicate care, attunement, and a gentle acknowledgment of distress. It can say, “I see you. I’m here. I’m not afraid of this.” When done slowly and without urgency, it can feel supportive without being intrusive.
It can also, unintentionally, communicate something else. “This is getting messy.” “Let’s clean this up.” “We should move on.” Not because the therapist means that, but because the client’s history may be primed to hear it.
Not handing a tissue can communicate spaciousness and trust. It can say, “You don’t need to stop. This is allowed.” It can convey confidence that the emotion can exist without intervention. For some clients, this feels deeply respectful.
For others, it feels like being left alone.
This is where therapists sometimes get stuck, looking for the “right” answer. Offer or don’t offer. Sooner or later. Hand it or place it nearby. Each option carries a different emotional weight depending on who is in the room.
The key is this. The tissue is not the intervention. The meaning of the gesture is.
Because therapists hold structural power in the room, even small gestures can carry disproportionate weight.
Clients rarely experience our actions in isolation. They experience them through the lens of their attachment history, cultural conditioning, and past moments of being overwhelmed with others. The tissue can unconsciously stand in for early caregivers. Who noticed. Who rushed in. Who withdrew. Who tolerated mess. Who didn’t.
This is why two clients can experience the same therapist behavior in completely different ways. One feels cared for. The other feels managed. One feels held. The other feels silenced.
None of this makes the therapist wrong. It makes the moment relational.
When therapists treat the tissue as a technical decision rather than a relational signal, we miss what’s actually happening. The client is not tracking the object. They are tracking us. Our pacing. Our body language. Our breath. Whether we seem grounded or uneasy. Whether we stay emotionally present or subtly pull away.
A tissue offered with steadiness lands differently than a tissue offered with haste. A tissue within reach lands differently than one placed into a client’s hand mid-sob. Silence paired with presence lands differently than silence paired with emotional distance.
The tissue simply amplifies what is already there.
Which brings us to a less comfortable but necessary place.
Because when a client cries, something also happens inside the therapist.
And that internal response matters more than the tissue ever will.
The Therapist’s Inner World When a Client Cries
When a client cries, the therapist’s nervous system responds too.
This often goes unnamed, but it is always there. A subtle tightening in the chest. A quickened internal pace. An urge to do something. Say something. Help. Fix. Reassure. Move the moment along so everyone can breathe again.
These impulses are human. They do not mean a therapist is unskilled or avoidant. They mean the therapist is in a room with real emotion and a relational responsibility.
What matters is not whether these impulses arise. What matters is whether we notice them.
For many therapists, crying activates a deep relational reflex. Comforting. Soothing. Rescuing. These instincts are not inherently wrong, but they are not neutral either. They are shaped by our own attachment histories, cultural conditioning, and experiences with helplessness. If we grew up being responsible for others’ emotions, tears may feel like a call to action. If we learned that strong emotion was overwhelming or dangerous, tears may trigger a desire to contain or redirect.
Sometimes the impulse is subtle. A reassuring phrase offered too quickly. A shift toward problem-solving. A gentle joke. A premature interpretation. None of these are inherently harmful. But when they arise reflexively, they can interrupt a process that was still unfolding.
There is also the therapist’s discomfort with not knowing what to do.
Crying exposes limits. It reminds us that we cannot take pain away on command. We cannot neatly organize grief, loss, or shame. The urge to act often masks a deeper discomfort with helplessness. Staying present without fixing asks us to tolerate our own vulnerability as witnesses.
This is where regulation begins.
A regulated therapist does not mean a detached one. It means a therapist who can notice their internal activation, slow it down, and choose a response rather than default to one. It means breathing before speaking. Letting silence do some of the work. Trusting the client’s nervous system rather than overriding it.
When therapists attend to their own internal experience in moments of client distress, they create space for attunement. They become less focused on managing the moment and more focused on being in it.
Clients feel this difference even if they cannot name it. They sense whether the therapist is comfortable enough to stay. Whether the therapist believes the emotion can be survived. Whether the therapist needs the tears to stop in order to feel competent.
This internal steadiness is what allows therapists to offer presence instead of performance. It is what makes any external gesture, including the tissue, land as supportive rather than corrective.
Once we understand that the therapist’s internal world shapes the moment, the next layer becomes clearer.
These moments are not just emotional. They are relational.
And in relationships, meaning is built in micro-moments.
Attachment Lives in Micro-Moments
Attachment is not built in grand gestures.
It is built in small, ordinary moments that quietly answer a single question again and again.
What happens when I am overwhelmed with you?
When a client cries, that question is no longer theoretical. It is embodied. The nervous system is watching closely, not for what you say, but for what you do. Do you stay. Do you rush. Do you tighten. Do you soften. Do you tolerate the intensity, or do you signal that it needs to be contained.
These moments become attachment data.
For clients with histories of emotional neglect, a therapist’s stillness may feel like familiar absence. For clients with histories of emotional intrusion, that same stillness may feel like respect and safety. For clients who learned that their feelings burdened others, a quick tissue handoff can register as pressure to clean up and move on. For clients who learned that no one ever noticed their pain, the absence of an offered tissue can feel like confirmation that they are alone again.
None of this is happening consciously.
Attachment lives below language. It is tracked through tone, timing, pacing, and presence. The nervous system is asking, often without words, “Can I feel this here?” and “Will you stay regulated if I don’t?”
This is why there is no universal rule about the tissue. The same action can communicate containment or rejection depending on the relational context. What matters is not the behavior itself, but whether the client experiences the therapist as emotionally available and unalarmed.
From an attachment perspective, the most important thing a therapist offers in moments of tears is not comfort or solutions. It is survivability. The quiet message that says, “This level of feeling can exist between us without something breaking.”
When a therapist stays grounded, unhurried, and present, they communicate that emotions do not threaten the relationship. They teach, through experience, that closeness does not require emotional tidiness.
This is especially powerful for clients who learned early that attachment came with conditions. Be calm. Be manageable. Be easy. Crying in therapy becomes a corrective emotional experience not because tears are encouraged, but because they are tolerated.
And when misattunement happens, because it always does, attachment does not require perfection. It requires responsiveness. The ability to notice, name, and repair.
These micro-moments are not tests to pass. They are invitations. Each one offers information about how this client experiences closeness, care, and vulnerability.
The tissue doesn’t create attachment.
Your presence does.
Presence Is an Intervention
In a culture that prizes action, productivity, and solutions, stillness can feel suspicious.
When a client cries, doing nothing can look like avoidance. Silence can feel awkward. Not reaching for words or gestures can trigger the fear that we are failing in our role. And yet, presence is not the absence of intervention. It is the intervention.
Presence is an active, embodied stance.
It is regulated breathing when emotion intensifies. It is staying oriented to the client rather than escaping into technique. It is allowing silence to hold what language would prematurely contain. It is trusting that the nervous system knows how to move through emotion when it is not rushed or redirected.
Presence requires more from the therapist than talking ever will.
It asks us to remain steady in the face of pain we cannot fix. To tolerate the discomfort of not rescuing. To resist the impulse to perform empathy instead of inhabiting it. Presence communicates safety not through explanation, but through nervous system resonance.
Clients feel this immediately. They sense whether the therapist is with them or managing them. Whether silence feels shared or abandoned. Whether the therapist’s stillness is grounded or frozen.
This is where many misunderstandings about therapy occur. Stillness without attunement can feel like withdrawal. Attunement without steadiness can feel intrusive. Presence lives in the balance between the two.
Simple phrases, offered sparingly and without urgency, can support presence without hijacking the moment. “I’m here.” “Take your time.” “We don’t need to rush this.” These statements do not close the emotional field. They keep it open.
When presence is strong, the need for action often decreases. The tissue becomes less charged. Words become optional rather than compulsory. The therapist’s body communicates what the client needs to hear.
Nothing about this is passive.
Presence is a skill that develops with practice, self-awareness, and a willingness to let go of the fantasy that we must always do something to be helpful. Sometimes the most therapeutic act is staying long enough for the nervous system to realize it is not alone.
And yet, even with presence, questions remain.
Because therapists still want to know.
Do I hand the tissue or not?
When Language Helps (And When It Waits)
Often, the most attuned response to tears is no language at all.
Stillness. Breath. Staying oriented. Letting the nervous system move without interruption.
And sometimes, once the wave has softened and the client feels resourced enough to reflect, language can gently open space rather than close it.
These are not scripts to deploy. They are examples of language that can support meaning-making when offered with appropriate timing, consent, and presence.
Used too early, even the gentlest words can pull a client out of their body and back into performance. Used too late, they may miss the moment entirely. Timing is the intervention.
Some options that tend to land softly when the client is ready:
“I’m here with you.”
Simple. Grounding. Often enough.
“We don’t need to rush this.”
A reminder that nothing needs to be fixed for the moment to be allowed.
“Take your time.”
Especially supportive for clients who learned to contain emotion quickly to protect others.
“Something feels important here.”
Naming significance without assigning meaning.
“What are your tears saying?”
For clients with enough reflective capacity, this question can invite meaning-making after the emotion has moved, as long as it’s offered without expectation or urgency.
“Do you want to stay with this, or shift a bit?”
An invitation that restores agency and choice.
“I’m noticing a lot of feeling here. How is it for you to let it be here right now?”
Centering the client’s experience rather than interpreting it.
What matters most is not the words themselves, but the stance behind them.
Language offered from curiosity feels different than language offered from discomfort. Language offered as an invitation feels different than language offered as a demand.
And sometimes, the most therapeutic response is saying nothing at all and staying.
Presence sets the conditions. Language follows, or doesn’t, depending on what the moment asks for.
So… Do You Hand the Tissue or Not?
Here’s the unsatisfying and honest answer.
Sometimes yes.
Sometimes no.
Sometimes later than you think you should.
Sometimes earlier than you meant to.
There is no universally correct moment, because the effectiveness of the gesture is not determined by the object. It’s determined by context.
What matters is not whether you offer a tissue, but how and why.
Context includes the client’s history with emotional expression. Their attachment patterns. Their cultural background. Their sensory needs. The phase of treatment. The intensity of the moment. The quality of the alliance. Even what just happened in the conversation before the tears arrived.
A tissue offered reflexively, the moment tears appear, can communicate urgency. It can signal “this needs to stop” even if that is not your intention. A tissue offered slowly, or placed within reach without commentary, often lands differently. It says, “Support is available, and you are not being rushed.”
For some clients, not offering a tissue immediately creates space. It allows the emotion to breathe before anything changes. For others, it feels like being unseen. Neither experience is wrong. Both are information.
This is where therapist attunement matters more than technique. Are you tracking the client, or your own discomfort? Are you responding to the moment, or to an internal rule about what therapists are “supposed” to do?
It can also help to remember that tissues do not have to be dramatic. They do not need to be handed ceremoniously, accompanied by reassurance, interpretation, or commentary. Often the most neutral option is simply ensuring tissues are accessible and letting the client decide if and when to reach for one.
Agency matters here.
The moment a client chooses to take a tissue themselves can be quietly empowering. It allows care without interruption. Support without intrusion.
And when you misjudge the moment, because you will, the work is not ruined. Which brings us to something therapists rarely say out loud but desperately need to hear.
When We Miss Each Other (And We Will)
Misattunement is not a failure of therapy. It is an inevitable feature of relationship.
You will offer a tissue when a client wished you hadn’t.
You will wait when a client hoped you’d step in.
You will say too much.
You will say too little.
What matters is not avoiding these moments. What matters is how you respond to them.
One of the most powerful clinical moves does not happen in the moment of tears, but later, when things have settled. Naming the experience gently. Inviting reflection. Restoring agency.
Something as simple as, “When you were crying earlier, I’m curious what that moment was like for you,” can open meaningful dialogue. It communicates that the client’s experience matters more than the therapist’s correctness. It models that relationships can be talked about rather than silently endured.
Repair is where trust deepens.
When therapists treat misattunement as catastrophic, they often become rigid. When they treat it as information, they remain flexible, responsive, and human. Clients do not need perfection. They need responsiveness.
And when repair is possible, even moments that felt awkward or painful can become part of the healing rather than evidence of failure.
Which leads us to the larger point this entire conversation has been circling.
What This Small Moment Teaches Us About Therapy
The tissue question is not really about tissues.
It is about how we relate to emotion.
How we tolerate vulnerability.
How we handle moments we cannot fix.
Therapy is not a place where feelings are optimized, managed, or made efficient. It is a place where emotions are allowed to exist without being rushed into meaning or resolution.
When a therapist can sit with tears without alarm, without performance, without urgency, they communicate something profound. That feelings are survivable. That vulnerability does not end relationships. That mess does not disqualify someone from care.
The smallest moments often carry the most weight. Not because they are dramatic, but because they are real.
A Reflection for the Therapist
You don’t need to answer these questions all at once. Let them sit with you. Let them surface in sessions, supervision, or the quiet moments between.
When a client cries, what happens first inside you?
Is there an impulse to act, to soothe, to explain, to move the moment along, or to stay very still?
What beliefs did you inherit about crying?
Who was allowed to cry in your world, and who was expected to stay composed?
When you imagine not intervening right away, what does that stir in you?
Discomfort, trust, fear, relief, or something else entirely?
How do you know when your response is coming from attunement rather than urgency?
What cues in your body help you tell the difference?
When misattunement happens, as it inevitably will, how do you tend to repair?
What helps you return to curiosity rather than self-criticism?
These moments are not tests of competence. They are invitations into deeper presence.
You don’t have to get them right.
You only have to stay.
A Closing Reflection for the Therapist Reading This
Clients will not remember whether you handed them a tissue at the “right” moment.
They will remember whether you stayed.
Whether you seemed afraid of their feelings or steady in their presence. Whether their vulnerability felt like a burden or something that could be held between two people without collapse.
Therapy is not perfected in technique. It is practiced in presence.
Sometimes that presence includes a tissue.
Sometimes it includes silence.
Often, it includes both.
What matters is not getting it right.
What matters is being there when it matters.
And that, quietly, is the work.

Written by Jen Hyatt, a licensed psychotherapist at Storm Haven Counseling & Wellness in Temecula, California.
Author’s Note
This piece grew out of a question that shows up again and again in therapy rooms, supervision spaces, and quiet therapist inner monologues. What do we do when a client cries? More specifically, do we hand them a tissue or not?
Rather than offering a rule or a “right answer,” this post explores what those moments actually hold. The nervous system shifts that happen during tears. The relational meaning carried by small gestures. The ways culture, attachment, and power quietly shape how care is experienced.
At The Nerdie Therapist, we believe therapy happens less in perfect interventions and more in human moments. This reflection is an invitation to slow down, stay curious, and trust presence over performance.
Read it not as instruction, but as orientation.
Disclaimer
This article is intended for educational and reflective purposes for mental health professionals. It does not constitute clinical, legal, or ethical advice, nor is it a substitute for supervision, consultation, or professional judgment. Therapists are encouraged to consider their scope of practice, training, and the specific needs of the clients they serve.





Leave a comment